 So it is important for all of us to understand the deadly E. coli bacteria, and take steps to prevent it from affecting us. Below is a brief summary of E. coli, along with answers to some frequently asked questions.
So it is important for all of us to understand the deadly E. coli bacteria, and take steps to prevent it from affecting us. Below is a brief summary of E. coli, along with answers to some frequently asked questions.E. coli Facts
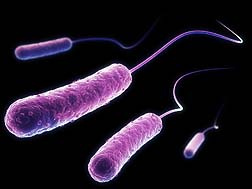
Escherichia coli (abbreviated as E. coli) are a very large and diverse group of bacteria that live in the intestinal tracts of warm blooded animals (predominantly cattle, pigs, goats, sheep, deer, and elk) and humans. The E. coli bacteria do not affect the animals - the animals are merely a carrier for the bacteria.
There are over 700 serotypes of E. coli. The most virulent of these produce shiga toxins and are called "shiga toxin-producing" E. coli, or STEC for short. They are sometimes referred to as verocytotoxic E. coli (VTEC) or enterohemorrhagic E. coli (EHEC). Shiga toxins are so named because they are virtually identical to those produced by another well known bacteria, i.e. shigella dysenteriae.
The most commonly identified STEC in North America is E. coli O157:H7 (often shortened to E. coli O157 or even just "O157"). When you hear news reports about outbreaks of "E. coli" infections, they are usually referring to E. coli O157.
In addition to E. coli O157, many other kinds (called serogroups) of STEC cause hemorrhagic colitis (bloody diarrhea). These other kinds are sometimes called "non-O157 STEC." E. coli serogroups O26, O111, and O103 are the non-O157 serogroups that most often cause illness in people in the United States. The non-O157 STEC are not nearly as well understood, partly because current protocols do not test for them and thus outbreaks due to them are rarely identified. As a whole, the non-O157 serogroup is less likely to cause severe illness than E. coli O157; however, some non-O157 STEC serogroups can cause the most severe manifestations.
STEC organisms are extremely virile - they can survive for weeks on surfaces such as kitchen counters and food preparation surfaces, and over a year within other materials. Unfortunately, a very small amount of E. coli in one's system can be deadly - the infectious dose of E. coli has been reported to be as few as 10 organisms.
E. coli O157:H7
The Center for Disease Control (CDC) first discovered E coli O157:H7 in 1975, although the bacteria was not implicated in food-borne illnesses until 1982 during an investigation into an outbreak of hemorrhagic colitis associated with contaminated hamburger.
Since 1982, more than 100 E. coli O157:H7 outbreaks have been detected in the United States. In actuality, that number is probably much higher because E. coli O157:H7 did not become a reportable disease (one that, upon detection by a lab, doctor, or hospital must be reported by law to local health officials ) until 1987.
The CDC estimates that every year over 73,000 are sickened, 2000 are hospitalized, and 60 die as a result of E. coli O157:H7 poisoning.
How is E. Coli transmitted?
The vast majority (reported 85 percent) of all E. coli illnesses are foodborne related (mostly ground beef). Inevitably, infections start when you swallow STEC—in other words, when you get tiny (usually invisible) amounts of human or animal feces in your mouth. Unfortunately, this happens more often than we would like to think about.
Although most E. coli illnesses are foodborne related, a small percentage have been tied to other transmission vehicles such as water, animals, ads person-to-person contact. People have become infected by swallowing lake water while swimming, touching the environment in petting zoos and other animal exhibits, and by eating food prepared by people who did not wash their hands well after using the toilet.
Who gets STEC infections?
People of any age can become infected. Very young children and the elderly are more likely to develop severe illness and hemolytic uremic syndrome (HUS) than others, but even healthy older children and young adults can become seriously ill.
What are the symptoms of STEC infections?
E. coli has emerged in recent years as the predominant cause of hemorrhagic colitis. This illness, with the characteristic symptoms of abdominal cramps and bloody diarrhea, can progress into a severe, life-threatening complication known as hemolytic uremic syndrome.
The symptoms of STEC infections vary for each person but often include severe stomach cramps, diarrhea (often bloody), and vomiting. If there is fever, it usually is not very high (less than 101ËšF/less than 38.5ËšC). Most people get better within 5–7 days. Some infections are very mild, but others are severe or even life-threatening.
What are the complications of STEC infections?
Around 5–10 percent of those who are diagnosed with STEC infection develop a potentially life-threatening complication known as hemolytic uremic syndrome (HUS). Clues that a person is developing HUS include decreased frequency of urination, feeling very tired, and losing pink color in cheeks and inside the lower eyelids. Persons with HUS should be hospitalized because their kidneys may stop working and they may develop other serious problems. Most persons with HUS recover within a few weeks, but some suffer permanent damage or die.
How soon do symptoms appear after exposure?
The time between ingesting the STEC bacteria and feeling sick is called the "incubation period." The incubation period is usually 3-4 days after the exposure, but may be as short as 1 day or as long as 10 days. The symptoms often begin slowly with mild belly pain or non-bloody diarrhea that worsens over several days. HUS, if it occurs, develops an average 7 days after the first symptoms, when the diarrhea is improving.
How are STEC infections diagnosed?
STEC infections are usually diagnosed through lab testing of stool specimens (feces). Identifying the specific strain of STEC involved is very important for public health purposes, such as finding outbreaks. Most labs can determine if an STEC is present and can identify E. coli O157. To determine the O group of non-O157 STEC, strains must be sent to a State Public Health laboratory.
What is the best treatment for STEC infection?
Non-specific supportive therapy, including hydration, is important. Antibiotics should not be used to treat this infection. There is no evidence that treatment with antibiotics is helpful, and taking antibiotics may increase the risk of HUS. Antidiarrheal agents like Imodium® may also increase that risk.
How can STEC infections be prevented?
1. WASH YOUR HANDS thoroughly after using the bathroom or changing diapers and before preparing or eating food.
2. WASH YOUR HANDS after contact with animals or their environments (at farms, petting zoos, fairs, even your own backyard).
READ MORE FOODBORNE ILLNESS LEGAL NEWS
4. AVOID raw milk, unpasteurized dairy products, and unpasteurized juices (like fresh apple cider).
5.AVOID swallowing water when swimming or playing in lakes, ponds, streams, swimming pools, and backyard "kiddie" pools.
6. PREVENT cross contamination in food preparation areas by thoroughly washing hands, counters, cutting boards, and utensils after they touch raw meat.
If you or a loved one have tested positive for E. coli you should contact a lawyer who can advise you on what steps can be taken to protect you and your family from the effects of this deadly bacteria.
